Why do I need a bypass operation to improve the blood supply to my leg?
The majority of patients with hardening of the arteries in the legs do not require surgery (see intermittent claudication). Most patients have a degree of disability which is manageable by adjustments in lifestyle, such as stopping smoking. Treating vascular risk factors reduces the risk of further problems due to atherosclerosis.
Hardening of the arteries in the legs only leads to serious problems in a small number of patients. However, if hardening of the arteries progresses, then there may be a risk of amputation.
Arterial bypass surgery is usually indicated in patients with a threatened leg due to lack of blood supply. In some of these cases, if left untreated, the limb may require amputation (critical limb ischaemia). It can also be considered in patients with very severe disabling claudication. Arterial bypass surgery can save the leg or reverse severe disability. The benefits of bypass surgery in patients with life style limiting claudication are more controversial. Many surgeons will advise against such surgery in these circumstances as surgery may precipitate problems as well as solve them.
Arterial bypass surgery is not minor surgery. Operations are frequently prolonged, complex and carry significant risks. The benefits and risks will be discussed with you by your vascular surgeon. . Bypass surgerywill l be the right option for many patients. In other patients an amputation may be more appropriate. In some very sick patients, with poor overall prognosis, the compassionate option may be to avoid any type of treatment and to allow the patient to die peacefully.
How will I know if my leg is in danger?
It is usually clear when the leg is in danger although an all embracing definition of critical leg ischaemia has been difficult to formulate. Most patients will experience at least one of the following symptoms:
Rest pain – this is a severe, continuous pain felt in the toes and foot. Some patients find that they only experience this pain at night. Many patients find that dangling the foot over the edge of the bed can help to ease the pain. The pain is often very severe, and patients will sleep in a chair to avoid the discomfort of elevating the leg. Gangrene – if the blood supply deteriorates to a stage where insufficient blood is available to keep the tissues alive then gangrene can develop, as shown (below right) in the 2nd toe (previous big toe amputation). This means that the tissue has died and turns black. If the tissues remain dry (mummified) then sometimes a toe can drop off without surgery. If it becomes wet (infected) then surgery is frequently required.

Ulceration and loss of tissue – sometimes frank gangrene does not develop but the tissues can develop sores called ulcers. . In this situation the skin tissues die and are shed leaving an ulcer crater which will not heal because the blood supply is so poor. This is shown in the picture (below left) in which an ulcer has developed on the outside of the foot due to a poor blood supply.

Severe disabling claudication – some patients experience none of the above symptoms but they can develop claudication symptoms after a few steps and managing a normal life becomes virtually impossible.
What will happen if I do not have an operation?
Amputation is the most likely outcome in patients with critical limb ischaemia (ulceration, gangrene, rest pain), who do not have bypass surgery to improve the blood supply to the leg. In patients with critical limb ischaemia, ulceration and gangrene will not resolve without some form of intervention. Improving the blood supply to the leg can allow healing to take place, but the gangrenous areas still need removal to enable healing to take place.
In patients with severe claudication, but no features of critical ischaemia, prediction of outcome can be difficult. Most surgeons would accept that bypass surgery is reasonable in these circumstances, if walking is becoming impossible even in the absence of gangrene, ulceration or rest pain. Without surgery, amputation is not inevitable. Many patients with severe claudication will merely continue with their symptoms and they may not deteriorate.
It must be acknowledged that there are patients in whom amputation may be the most appropriate way forward. There are many reasons for this, but the potential benefits of the operation for any individual must always be balanced against the potential risks and complications.
Should I stop smoking before the operation?
Every patient with hardening of the arteries should stop smoking. Simply decreasing smoking is unlikely to produce any benefit. Continuing to smoke is almost certain to produce a worsening of arterial disease. The effects of smoking are cumulative and take time.
Damage produced by smoking continuously over many years cannot be undone by suddenly stopping smoking. However, even stopping smoking for a relatively short period before operation or angioplasty may reduce your risks of the procedure failing or leading to complications. Continued smoking after lower limb bypass surgery results in a threefold increased risk of the bypass graft blocking off. (Willigendael EM et al, 2005).
What tests will I have before surgery?
Workup will include detailed history and examination. This will pay particular attention to previous vascular disease, previous bypass surgery, medications and heart and lung function.
Various radiology imaging techniques will be performed to provide your surgeon with a roadmap of the arteries. This can include ultrasounds, CT scans and MRI scans. Sometimes an angiogram is performed via a needle puncture in the groin under local anaesthetic. Your kidney function will be assessed by blood tests, prior to some of these scans. The dye used during the radiology tests can be damaging to your kidneys if they are not working well, and this will be considered carefully by your surgeon. This detailed information will tell the surgeon whether bypass surgery is likely to be beneficial and will permit detailed planning of any bypass that is possible. A roadmap of the veins in the leg using ultrasound is also often useful as the veins can be used to provide a channel to take blood to the arteries lower down the leg.
Sometimes, a small balloon inside your arteries can open up a narrowing to improve the blood flow to the foot. This is called angioplasty and is also performed via a needle in the groin, under local anaesthesia. A splint called a stent is sometimes used to hold the artery open as well. . This option may not be possible if the arterial disease is more extensive and spans 2 or 3 levels. Your surgeon will decide whether angioplasty is attempted or not. Angioplasty is often done in combination with bypass surgery. All of these options have risks and complications, that will be discussed with you.
How do bypass operations work?
The essential problem in all patients undergoing bypass surgery to the lower legs is that insufficient blood and hence oxygen is able to reach the tissues of the leg and foot. The tissues are starved of oxygen and this is what leads to pain, gangrene and ulceration.
Bypass operations work by improving the blood supply and hence the oxygen supply to the tissues that have been starved of oxygen. To do this the surgeon must take blood from a good artery above the area where the artery is blocked, and take the blood along a tube (the conduit) to a good artery below the blocked segments.
There are variations on this principle when blood can be taken from one side of the body to the other (femoro-femoral crossover) or blood is diverted from arteries to the arms down to the legs (axillo-bifemoral grafting).
What operation will be performed?
Inflow operations
Inflow operations are performed to restore blood flow to the top of the leg. When the blood flow is normal to the legs, pulses can be felt around the groin area. If major blood vessels (aorta or iliac arteries) are blocked then the blood flowing into the leg is severely reduced. An inflow operation is required to restore this flow to normal.
 There are many operations to restore inflow to the legs, but the commonest are:
There are many operations to restore inflow to the legs, but the commonest are:
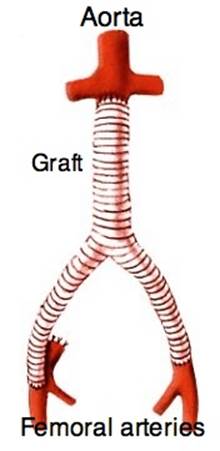
Aorto bifemoral grafting – (left) these grafts originate on the aorta (main artery in the abdomen) and take blood to the femoral arteries at the groins. These are major operations with an approximately 3-5% (1 in 20) risk of dying. Aorto-bifemoral grafting is the most successful type of inflow operation, but is also the most traumatic. Aman made graft is stitched to the aorta in the abdomen, just below the level of the kidneys. The graft has two legs which are then tunnelled under the abdominal muscles into the groins to be attached to the femoral arteries. A diagram of an aorto-bifemoral graft is shown on the left.
Axillobifemoral grafting – these grafts originate from the axillary arteries (supplying the arms) just below the collar bones and take blood to the femoral arteries. This is sometimes the best option in very elderly or very unfit patients as it is a less traumatic alternative to aorto-bifemoral grafting.
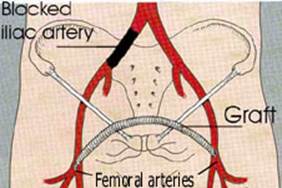
Femoro-femoral cross-over grafting – (below right) these grafts originate from a normal femoral artery in the groin on one leg and take blood to the femoral artery in the groin on the opposite leg. In the example shown below right a graft is running from the left femoral artery in the patient to the right femoral artery. At least one of the arteries running to the legs must be flowing normally in order to perform this operation.
Ilio-femoral bypass grafting – these grafts originate from the iliac arteries in the pelvis and take blood to the femoral arteries in the groins. These can be useful if there is enough normal iliac artery in the pelvis.
The common theme with these operations is that they restore good blood flow to the femoral artery at the top of the leg in the groin region. Restoring the inflow to normal levels is often all that is required in many patients, even if there is disease in the arteries further down the leg. The improvement in inflow alone can be enough to permit healing or reduce symptoms to a more bearable level.
Outflow operations
If the arterial flow to the femoral artery is good and there are good femoral pulses in the groin, an inflow operation is not required. If the patient has a shortage of blood to the leg and good femoral pulses then the arterial problem must lie at a lower level in the thigh and/or the calf arteries. These operations are frequently prolonged and complex procedures and best results are obtained by using vein grafts if possible. There are many operations to restore blood flow to the legs, but the commonest are:

Femoro-popliteal bypass
These grafts originate from the femoral artery in the groin and take blood to the popliteal artery either just above or below the knee. Femoro-distal or femoro-crural bypass – these grafts originate from the femoral artery at the groin and take blood to one of the 3 calf blood vessels (anterior and posterior tibial arteries and peroneal artery). The picture below shows the appearance of the leg following a femoro-peroneal bypass. This patient also required amputation of toes.
Pedal bypasses
These grafts can originate from any artery in the leg (femoral, popliteal and rarely tibial) and take blood to arteries below the level of the ankle joint (dorsalis pedis artery and posterior tibial artery or their branchesFemoral endarterectomy in which the diseased lining of the artery can be removed and blood flow restored.
General graft principles
For inflow operations it is better to use artificial/man made grafts. They perform well when the arterial flow is high and have been shown over years to provide durable results.
For outflow operations it is better to use veins harvested from the leg as the conduit or tube to take blood.These veins are also used in patients having heart bypass operations. Sometimes artificial/man madematerials have to be used as no vein is available. .
The grafts are stitched to the arteries using fine polypropylene stitches (similar to nylon). Permanent stitches are used because the joins between the grafts and the native artery require lifelong support. What types of anaesthetic are used?
Bypass surgery is frequently time consuming and complicated. General anaesthesia where the patient is asleep and unconscious throughout the operation is probably the commonest form of anaesthesia used. On other occasions, epidural blocks or local anesthesia may be used. This will be discussed with you by the anesthetist and surgeon. Options can vary depending on the site of the operation and your overall health.
What are the complications of bypass surgery?
Complications of any operation can be divided into local and general.
Local complications
Graft failure – the bypass graft may block and the blood supply to the leg and foot will be reduced to the levels that were present before the bypass surgery. In fact on many occasions when a bypass graft blocks, especially in the early period (hours to weeks) after surgery, the blood supply can be worse than before the bypass surgery. In these circumstances amputation can be inevitable unless the graft can be salvaged and the blood supply restored.
Wound infection – wound infections arecommon in vascular bypass surgery in the leg due to a combination of factors.. Minor wound infections are usually treatable by a combination of dressings, antibiotics and sometimes drainage of infection.
Graft infection – if the infection involves the graft, the situation is very much more serious. It is frequently impossible to eradicate infection from artificial materials and they need to be removed. When this happens the blood flow down the bypass graft is also removed. Unless an alternative route for a bypass graft can be found, this situation will frequently end in amputation. Graft infection is fortunately uncommon, probably only affecting about 5% of man made grafts. The presence of infection around a vein graft is more controllable and less likely to end in serious consequences.
Leg swelling – this is a very common event after lower limb bypass surgery. It is due to a combination of factors. Much of it may resolve, but not completely.
General complications
Chest infections, heart attacks and strokes – because bypass surgery is prolonged and frequently takes place in elderly patients with other significant problems, these complications are not uncommon. Will I need further treatment after my operation?
All patients with hardening of the arteries should take a small dose of aspirin every day. Aspirin changes with the blood making clots less likely to form. Other alternatives to thin the blood may be used. These can include Plavix (clopidogrel) and warfarin. . If you are taking warfarin tablets it is important that you have regular blood coagulation tests to monitor how well the warfarin is working and ensure that it is kept under control. Almost all patients will be prescribed cholesterol lowering medication which has multiple benefits for patients with hardening of the arteries.
In addition, your vascular risk factors such as high blood pressure should be treated.
Ultrasound surveillance
In about one third of grafts performed with veins a narrowing develops after the operation. To identify patients who develop narrowing, Ultrasound scanning of the graft is usually recommended at frequent intervals over the first two years. This enables problems to be identified at an early stage when they can be corrected before the graft blocks. Once a graft blocks it is usually more difficult to rescue the situation and restore normal blood flow. What are the results of bypass surgery?
The results of bypass surgery vary enormously depending on the type of graft (artificial or vein graft) inserted, the severity of the arterial disease and the site of the graft. The larger grafts taking blood to the femoral arteries at the groin have rates of 70-90% functioning normally at 5 years after surgery.
The results of surgery below the groin are not as good but your individual case will be discussed with you.
Useful links
http://www.surgeryencyclopedia.com/Pa-St/Peripheral-Vascular-Bypass-Surgery.html
http://www.cochrane.org/reviews/en/ab001487.html
www.emedicine.com/med/topic2776.htm – Detailed information on upper limb vascular disease. This is much less common disease with little information on the internet.
http://c561949.r49.cf2.rackcdn.com/videos/SVS_Conte_LEBypass.wmv – Podcast information from the Society of Vascular Surgery in the USA
http://www.vascularweb.org/vascularhealth/Pages/surgical-bypass.aspxA
http://www.nhs.uk/Conditions/Gangrene/Pages/new_Treatment.aspx
References
Willingendael EM, Teijink JAW, Bartelink ML et al.Smoking and the patency of lower extremity bypass grafts: a meta-analysis. J Vasc Surg 2005; 42: 67-74.
Pursell R, Sideso E, Magee T, Galland RB. Critical appraisal of femorofemoral crossover grafts. Brit J Surg 2005; 92: 565-69.
Basil Trial Participants.Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 2005; 366: 1925-34.
Johnson WC, Williford WO, et al. Benefits, morbidity, and mortality associated with long-term administration of oral anticoagulant therapy to patients with peripheral arterial bypass procedures: a prospective randomized study. J Vasc Surg 2001; 35: 413-21.
Pereira CE, Albers M, Romiti M, Neto F, Pereira CA. Meta-analysis of femoropopliteal bypass grafts for lower extremity arterial insufficiency. J Vasc Surg 2006; 44: 510-7.
Takagi H, Goto S, Matsui M, Manabe H, Umemoto T. A contemporary meta-analysis of Dacron versus polytetrafluoroethylene grafts for femoropopliteal bypass grafting. J Vasc Surg 2010; 52: 232-6.
van Det, Vriens BHR, van der Palen J, Geelkerken RH. Dacron or ePTFE for femoro-popliteal above-knee bypass grafting: short- and long-term results of a multicentre randomised trial. Eur J Vasc Endovasc Surg 2009; 37: 457-463.
Nicoloff AD, Taylor LM, McLafferty RB, Moneta GL, Porter JM. Patient recovery after infrainguinal bypass grafting for limb salvage. J Vasc Surg 1998; 27: 256-66.
